1601006195 SHORT CASE
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment"
FAMILY HISTORY
GENERAL MEDICINE SHORT CASE
HT.No 1601006195
A 55 year old male from miryalguda labourer by occupation came to opd with chief complaints of
1.PAIN Abdomen since 15 days
2.FEVER for 12 days
History of presenting illness:
patient was apparently asymptomatic 15 days back and then he developed
severe pain in the right upper quadrant which was sudden in onset, gradually progressive,dragging type and non radiating
aggravated on standing position and relieved by medications and not associated with nausea and vomiting and loose stools and
then later he developed
fever since 12 days which was high-grade and continuous and associated with chills and rigors for one day and not associated with the cold and cough shortness of breath headache dizziness and vomiting
No history of chest pain palpitation burning micturition
Past history
no similar complaints in the past not a known case of diabetes mellitus hypertension,asthma and epilepsy and tuberculosis
PERSONAL HISTORY
appetite decreased since one week
diet mixed
bowel and bladder - regular
no burning micturition
he is a toddy drinker since 30 years
He smokes 10 beedis per day since 30 years
There is no significant family
General examination
Patient was conscious coherent and cooperative sitting comfortable on the bed
He is well oriented to time place and person
moderately built and moderately Nourished
Icterus is present
No signs of pallor clubbing cyanosis and generalized lymphadenopathy
VITALS
Pulse 78 beats /min regular normal value and character there is no radio radial and radio femoral delay
Blood pressure 110 /80 mmHg left arm in supine position
Respiratory rate 16 cycles per minute
JVP normal
Temperature : Afebrile
FEVER CHART
SYSTEMIC EXAMINATION
CVS S1 S2 heard no murmurs
Respiratory system examination decreased air entry,bilateral fine crepitations are present in right lower lobe and left lower lobe
ABDOMINAL EXAMINATION
INSPECTION
Shape of the abdomen flat
Umbilicus : normal
no visible pulsation
no visible peristalsis
all quadrants of abdomen moving equal with respiration
PALPATION
Inspectory findings are confirmed
No local rise of temperature tenderness is present over the right hypochondrium right upper quadrant no palpable mass
Liver and spleen or not palpable
PERCUSSION
liver span is normal
AUSCULATION
bowels sounds are heard
Provisional diagnosis:LIVER ABSCESS
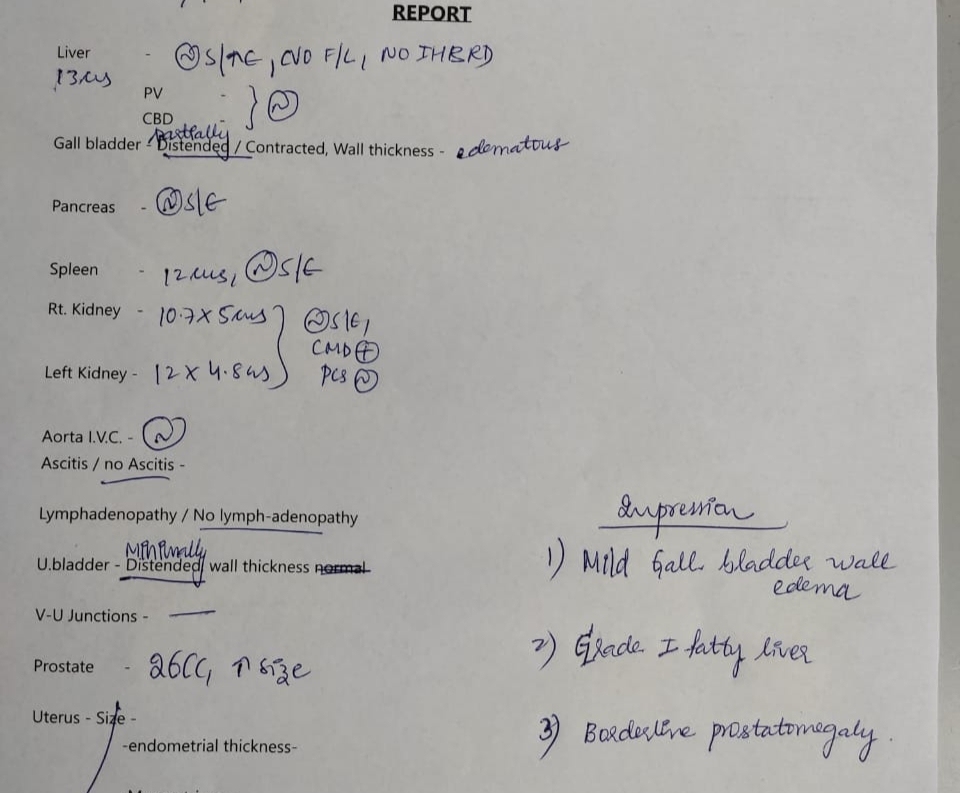
INVESTIGATIONS
HEMOGRAM reduced hemoglobin
Reduced lymphocytes
Renal function test:
TREATMENT:
1.THIAMINE INJECTION
2.CLINDAMYCIN PHOSPHATE 600mg
3.TRAMODOL HCL
4.AMPICILLIN and CLOXACILLIN
5.PANTOPRAZOLE INJECTION









Comments
Post a Comment